Projects
-
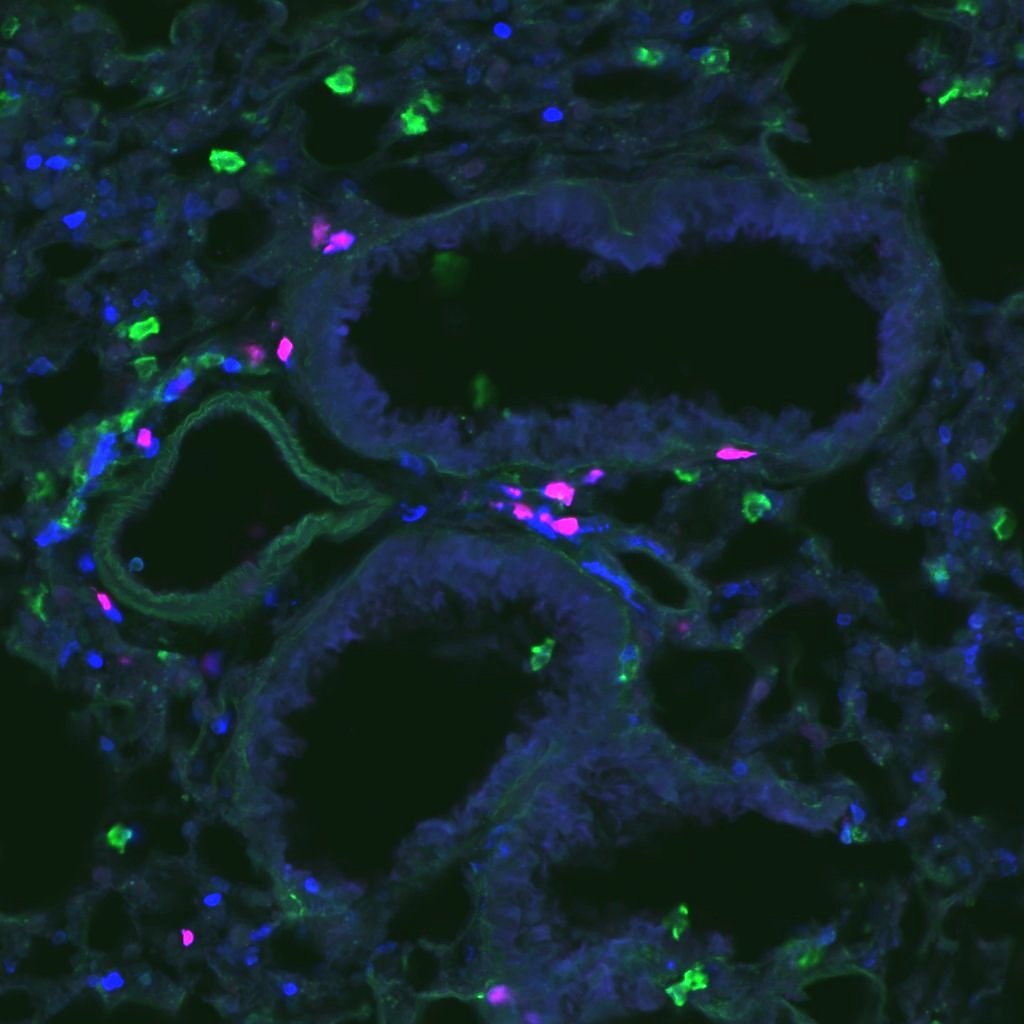
The induction of allergen-specific Th2 cells and IgE are required for the development of allergic disease, but allergic individuals can exhibit disease involvement at distinct barrier surfaces. Specifically, individuals with allergen-specific Th2 cells and IgE against ubiquitous aeroallergens can exhibit skin or airway involvement. Such observations demonstrate that systemic sensitization and development of allergen-specific type 2 immunity is necessary, but not sufficient for disease development. Our group and others have shown that memory Th2 cells can establish long-term residency in the lungs to drive recurrent allergic airway disease, suggesting that local adaptive type 2 immunity is critical to promote tissue-specific allergic disease. We are defining the rules that regulate the development of tissue-resident memory Th2 cells in barrier tissues with a focus on how distinct antigen presenting cells within barrier tissues regulate Th2 cell fate.
-
FoxP3+ regulatory T cells (Tregs) are critical in maintaining tolerance to self and environmental antigens as well as modulating immune responses. In humans, mutations in genes critical for Treg function lead to the development of allergic disease. Howtver, the mechanisms whereby Tregs restrain type 2 immunity remain unclear. We are defining the mechanisms whereby Tregs survey and restrain Th2-promoting dendritic cells in the lungs and lung-draining lymph nodes. Identifying the mechanisms of Treg suppression of type 2 immunity has the potential to nominate new therapeutic approaches to suppress chronic allergic disease.
